Diabetic retinopathy is a serious eye disease that affects more than six million Americans and is one of the
Trusted Source
Diabetic Retinopathy Data and Statistics
National Eye Institute
Go to Source
most common causes of vision loss in adults
under the age of 60. Without proper treatment, diabetic retinopathy can cause blindness. The ophthalmologists at Retina Specialty Institute are extensively trained in the treatment of diabetic retinopathy and can help residents of Alabama, Florida, Mississippi, and the Gulf Coast region preserve and protect their sight.
What is Diabetic Retinopathy?
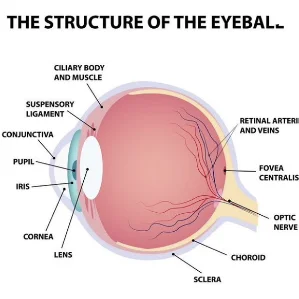
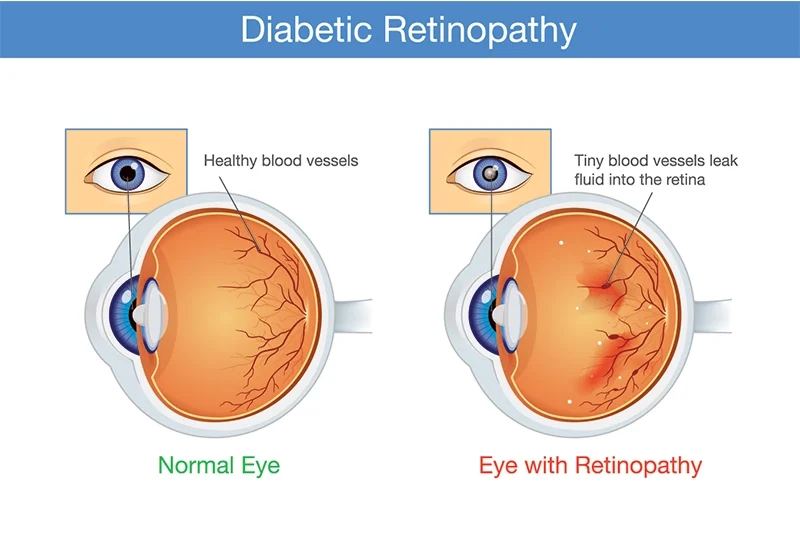
The retina is a layer of tissue at the back of the eye, and it is made of cells that are sensitive to light. The retina processes light so that the optic nerve can produce visual images. In patients with diabetes, high blood sugar levels can cause damage to tiny blood vessels located in the retina, eliminating their blood supply. Over time, the eye grows new blood vessels, but these new vessels aren’t properly developed and may leak.
Diabetic Retinopathy Risk Factors
The Centers for Disease Control and Prevention states that the
Trusted Source
Diabetes and Vision Loss
Centers for Disease Control and Prevention
Go to Source
risk for diabetic retinopathy increases
the longer a person lives with diabetes. This condition is a threat for people with Type 1 diabetes, Type 2 diabetes, and gestational diabetes. Additional factors that increase the risk of diabetic retinopathy include:
- Uncontrolled blood sugar
- High cholesterol
- High blood pressure
- Latino/Hispanic or African-American heritage

Symptoms of Diabetic Retinopathy
Early stages of diabetic retinopathy are often asymptomatic, so it is important to see your eye doctor regularly if you have diabetes. Symptoms of diabetic retinopathy include:
- Increase in floaters
- Trouble seeing in low light
- Dark spots or blind spots in your vision
- Blurry vision
-
Trusted Source Diabetic Retinopathy Mayo Clinic Go to Source Changes in your near or distant vision
Types or Stages of Diabetic Retinopathy
The stages of diabetic retinopathy include:
Non-Proliferative Diabetic Retinopathy (NPDR)
In this early stage of diabetic retinopathy, circulation of blood to the retina is compromised by blood vessels that swell and leak. Patients commonly encounter retinal hemorrhages and microaneurysms. Treatment may not be necessary at this early diabetic retinopathy stage, but patients should be closely monitored by an eye doctor so that prompt treatment can be rendered when necessary.
Proliferative Diabetic Retinopathy (PDR)
Proliferative diabetic retinopathy is the most severe stage of this condition. PDR occurs when the eye attempts to grow new blood vessels to feed the retina. These new blood vessels are abnormal, and they often break and leak. This complication is called vitreous hemorrhage. Additional complications of proliferative diabetic retinopathy may include retinal scarring, death of retinal nerve cells, and retinal detachment. This advanced stage of diabetic retinopathy can cause eye pain, dark spots, an increase in floaters, and potential permanent vision loss.
Complications of Diabetic Retinopathy
There are several complications of diabetic retinopathy that can compromise a patient’s vision, including:
Diabetic Macular Edema (DME)
Diabetic macular edema occurs at a stage of diabetic retinopathy where the blood vessels in the eye have been damaged to the extent that they begin to leak. This causes blurry vision and swelling of the retina, and can cause vision loss if left untreated.
Vitreous Hemorrhage
The vitreous is the clear, jelly-like substance in the center of the eye. When new, abnormal blood cells grow on the surface of a retina affected by diabetic retinopathy, they may rupture or leak, leading to a vitreous hemorrhage. A large vitreous hemorrhage can block portions or all of the patient’s vision. This may resolve over the course of days or months, but if it takes too long to resolve surgery (vitrectomy) may be necessary.
Traction Retinal Detachment
In patients at the proliferative stage of diabetic retinopathy, scar tissue can cause the retina to wrinkle, shrink, or pull out of position. This can cause visual distortion or even severe vision loss.
Neovascular Glaucoma
In some cases of advanced diabetic retinopathy, the eye may grow new, abnormal blood vessels on the iris. This can block the flow of fluid out of the eye, increasing eye pressure and leading to neovascular glaucoma. This is a painful and severe eye disease that can cause optic nerve damage.

Treatment for Diabetic Retinopathy
According to the American Academy of Ophthalmology, up to 90% of diabetic retinopathy vision loss can be
Trusted Source
Diabetic Eye Disease
American Academy of Ophthalmology
Go to Source
prevented with proper treatment
. Treatment of early diabetic eye disease may consist of helping the patient manage their blood sugar through dietary changes and exercise.
In addition to encouraging you to manage your blood sugar, your eye doctor may also prescribe medication to reduce swelling in your retina.
In cases where abnormal or leaking blood vessels are present, your doctor may perform laser surgery to seal leaking vessels off or shrink them. Your eye doctor may also perform intraocular injections with steroids and/or anti-VEGF medications.
If diabetic retinopathy has caused a vitreous hemorrhage, your eye doctor may perform a vitrectomy. This is a microsurgical procedure during which vitreous that is full of blood is removed and replaced with a clear solution. A detached retina can also be repaired during vitrectomy.
Frequently Asked Questions About Diabetic Retinopathy
When should I schedule an eye examination?
Like many eye conditions, diabetic retinopathy is best treated at its early stages, when patients may not notice symptoms. This is why it is so important to see your eye doctor for regular eye exams, especially if you have diabetes.
How is diabetic retinopathy diagnosed?
Early diagnosis is key to preventing vision loss from diabetic retinopathy. Your eye doctor can diagnose diabetic retinopathy through an examination of the retina at the back of the eye. Additional diagnostic tests such as fluorescein angiography (FA) and/or optical coherence tomography (OCT) may be performed to detect abnormalities in the blood vessels that nourish the retina.
Can diabetic retinopathy be prevented?
You may be able to decrease your risk of diabetic retinopathy or even prevent this condition by controlling your blood sugar, taking certain medications, and following a healthy diet and exercise routine.

Contact Retina Specialty Institute
At Retina Specialty Institute, our ophthalmologists have expert training and considerable experience in the early diagnosis and treatment of diabetic retinopathy.
1 National Eye Institute. Diabetic Retinopathy Data and Statistics. Available: https://www.nei.nih.gov/learn-about-eye-health/outreach-campaigns-and-resources/eye-health-data-and-statistics/diabetic-Retinopathy-data-and-statistics Accessed August 2, 2022.
2 Mayo Clinic. Diabetic Retinopathy. Available: https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611. Accessed August 2, 2022.
3 Centers for Disease Control and Prevention. Diabetes and Vision Loss. Available: https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-vision-loss.html?CDC_AAref_Val Accessed September 20, 2024.
4 American Academy of Ophthalmology. Diabetic Eye Disease. Available: https://www.aao.org/eye-health/diseases/diabetic-eye-disease Accessed August 2, 2022.
The doctors at Retina Specialty Institute have either authored or reviewed and approved this content.
Page Updated: